Value-based reimbursement models and Medicare Advantage plans continue to gain momentum. Is your organization built to handle the growth of value-based contracts?
If not, a scalable HCC coding infrastructure can help. Successful HCC coding leads to accurate RAF scores and ensures your organization has the revenue necessary to continue providing high-quality patient care. A scalable HCC coding infrastructure is one that can smoothly handle increasing numbers of patients over time, as more of your patients move into ACOs or risk-based contracts.
To start building your own scalable HCC coding infrastructure, we recommend these three best practices:
1. Leverage Your Current EHR and RCM System Workflows
Healthcare organizations must ensure that clinical documentation in the EHR is accurately reported to the payers in the form of a claim. This is true in both the fee-for-service world as well as the HCC coding world.
In the fee-for-service world, leading healthcare organizations have implemented claim scrubbers and a coding review process to ensure claims are administratively accurate before submitting them to a payer. This proven process has been in place for decades.
This same process can be implemented for HCC coding. This will ensure that high-value encounters (such as patients with multiple chronic conditions and a potentially high RAF value) are reviewed by coders before initial claim submission. Using a process very similar to your time-proven revenue cycle approach, your organization can build a value-based claim review process that works in parallel with your existing fee-for-service process.
2. Value Your HCC Coders
Nursing and physician shortages aren't the only staffing challenges facing providers today. According to a STAT poll from the Medical Group Management Association, many healthcare organizations report they can't find enough qualified coders.1
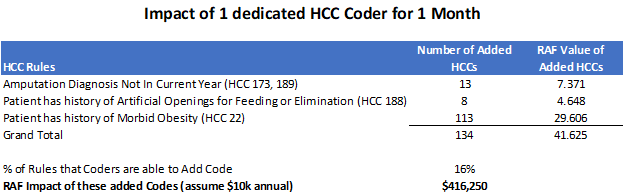
The need for certified risk coders (CRCs) is particularly acute, as they are essential to achieving financial success under value-based contracts. The good news is that you can start small and scale over time. Even adding a single HCC coder to your team can have impressive results. In the example below, a health system in Florida took this exact approach. They hired a single HCC coder and focused on three foundational HCC conditions. With a single coder and this narrow focus, they were still able to increase RAF value by over $416K in one month.
3. Implement HCC Coding Technology to Increase Productivity and Efficiency
Because HCC coders are expensive and difficult to find, very few physician groups can afford to hire certified coders to review every encounter. As a result, it is critical to maximize coders’ efficiency and productivity.
One way to achieve this is to partner with technology companies that can automatically identify high-value HCC claims for coder review. This allows a small group of coders to cover a large number of physicians, making it far easier—and much more cost-effective—to scale up as your value-based volume increases.
Our customers’ experience is that a seasoned risk coder can work between 40 to 60 encounters per day. The key is to ensure they focus on the highest value encounters. Filtering value-based claims by payer, provider, and specific chronic condition(s) ensures that your coders are working the high-value encounters, while not being overwhelmed by the volume.
In the example above, the organization had limited resources and needed to prioritize their single HCC coder’s time to guarantee the best return on their investment (ROI). With their combined investment in an HCC coder and HCC coding technology, this organization achieved a sizable return on their investment.
Sources: