You may already be familiar with Claim Scrubbers. But did you know that claim scrubbers are no longer the only option for a practice looking to increase their claim processing accuracy and efficiency? Charge Scrubbers are another helpful, error-flagging alternative to consider for your claim editing needs. In this post, we’ll detail more about each of these offerings and their unique benefits, so that you can make the right call for your organization.
Claim Scrubbers vs. Charge Scrubbers
Before we get into how they compare, let’s start with some basic definitions:
What is a Claim Scrubber?
Claim Scrubbers review medical claims for coding and billing accuracy. This claim data review takes place after a claim is created in the RCM system but before going to the payer. If the Claim Scrubber identifies an error, a task is typically created for a biller or coder to work within the RCM tasking system. In many cases the coder or biller will make the correction(s) and then repost it into the RCM system, accurate and error-free.
What is a Charge Scrubber?
Charge Scrubbers identify medical coding and billing issues as well, but this solution reviews charges before the charge enters the RCM system. If the Charge Scrubber identifies an error, it is flagged so that a coder or biller can make the corrections before a claim is created. In this model, the scrubbed charges enter the RCM system accurate and ready to be submitted as a claim.
Benefits of each option
Both scrubbing options help you identify errors and save you from having to deal with clearinghouse rejections, payer denials and other back-end re-work. They share many of the same features and benefits which include automating the review of charges and claims against a comprehensive library of edits, and automating the distribution of work via tasking. In most cases, both products offer the ability to create custom rules that accommodate various payer and reimbursement guidelines. Both are great options for improving key metrics such as efficiency and cash flow.
As discussed above, the primary difference between the two Scrubbers is where and when the scrubbing takes place. While Claim Scrubbers work on the back-end of the process, post-claim creation, Charge Scrubbers focus on the front-end of the process, pre-claim creation. Claim Scrubbers offer the unique benefits of being able to work tasks within the RCM system, while also offering secondary and tertiary claim processing capabilities. On the other hand, Charge Scrubbers help you get ahead of the problem by flagging issues before a claim is created, and some, such as the RCxRules software, can even help autocorrect common coding and billing errors for extra-efficiency. For example, with RCxRules you can automatically add administration/injection codes, add/remove modifiers and re-order CPT and DX codes.
Solution Comparison Chart
See the chart below to find out how the features and benefits of both scrubbers compare:
Feature/Benefit |
Claim Scrubber |
Charge Scrubber |
| Less burden on providers to code correctly |  |
 |
| Reduced denials |  |
 |
| Improved cash flow |  |
 |
| Reduced manual work due to automated tasking |  |
 |
| Less days in A/R |  |
 |
| Tasks worked in RCM system |  |
|
| Process secondary/tertiary claims |  |
|
| Includes HCC coding rules |  |
 |
| Front-end review process: Charges are corrected before a claim is created |  |
|
| Autocorrect common coding/billing errors |  |
|
| Create custom rules specific to your payers and specialty |  |
 |
Which scrubber software is right for you?
Fortunately, it’s hard to go wrong with either of these options. Both the Claim Scrubber and the Charge Scrubber software help you ensure clean claims the first time. The best option for you is the one that works most seamlessly and effectively within your current processes and systems. And whichever model you select, RCxRules can help ensure it’s a success.
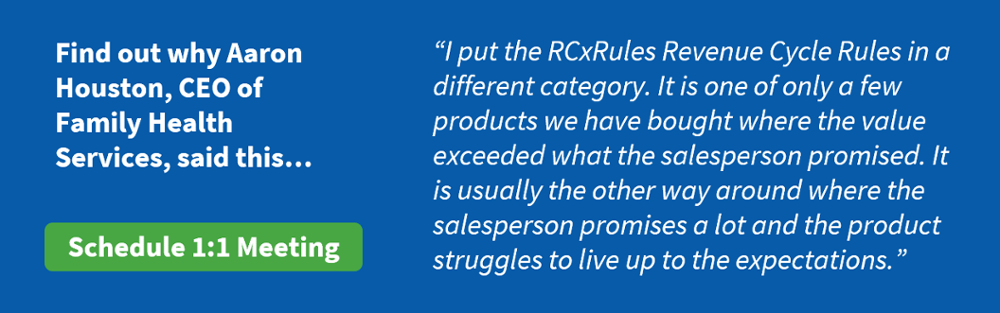
To learn more about Claim and Charge Scrubbers, and to discuss which software would be the best fit for your unique organization, reach out to set up a meeting today.